 |


|
|
CD4 (T-Cell) Counts, and Viral Load |
|
Although these forces sometimes accept the need to treat opportunistic infections, most reject the vast majority of conventional HIV/AIDS treatment, especially use of drugs to combat HIV. This article is part of a series in which AIDS Treatment News examines key arguments put forth by the "dissidents"--perhaps more accurately termed "AIDS denialists," because most deny that AIDS is a genuine epidemic and many deny that the term "AIDS" even describes a real medical condition. The AIDS denialist movement is not unified (for example, some groups say that HIV is a harmless virus, while others say HIV does not exist), so the summary here of some of their arguments is necessarily only a sketch. More detailed descriptions can be found in the references listed below. Answering Denialist Views on CD4 (T-Cell) Tests One consistent thread running through the denialist literature is the assertion that AIDS medicine has made a serious mistake by relying on laboratory markers such as CD4 cell counts, and viral load as measured by techniques such as polymerase chain reaction (PCR). These markers are criticized as unreliable at best and a devious effort to hide the failure of HIV/AIDS science at worst. One recently-formed group, ACT UP Hollywood (not connected with long-standing ACT UP chapters in New York, Philadelphia and elsewhere), argues that "all HIV and viral load tests as well as T-cell counts need to be banned immediately because they are useless indicators of a person's health."(1)
The denialist argument appears to be built upon a narrow and highly selective reading of the data. For example one of the sources Maggiore cites as proof for the above statement that low CD4 counts can occur without HIV, a Transfusion Safety Study Group report at the 9th International AIDS Conference, specifically notes that HIV-negative individuals with two or more CD4 counts below 300 were rare, and that both those with known and unknown causes of immune suppression "differ from the retrovirus immunodeficiency pattern" in a number of key parameters, including CD4 percentage and CD4/CD8 ratio.(5) In other words, transient low CD4 counts seen in other circumstances do not equal AIDS and bear little resemblance to what is typically seen in HIV-infected individuals. What the denialists regularly ignore is that while unusually low CD4 counts can occur for a variety of reasons, numerous large, long-term cohort studies have demonstrated a distinct pattern associated with HIV infection: A statistically significant CD4 decline commonly begins around the time of seroconversion and gradually becomes more severe over time, eventually leading to increased susceptibility to opportunistic infections. This has been observed in cohorts of gay men, transfusion recipients and hemophiliacs. In these cohorts a decline in CD4 count has been consistently and strongly associated with the development of AIDS-defining illnesses.(6) Also neglected in denialist discussions of CD4 is the large body of evidence associating specific opportunistic infections with lowered CD4 counts. For example, in the Pulmonary Complications of HIV Study, an 1,182-person cohort, 79 percent of cases of pneumocystis carinii pneumonia (PCP) occurred in individuals with CD4 counts below 100 and 95 percent occurred in patients whose CD4 count was below 200.(7)
 Members of ACT UP/San Francisco storm the offices of the AIDS organization Project Inform
Members of ACT UP/San Francisco storm the offices of the AIDS organization Project Inform
The Multicenter AIDS Cohort Study (MACS) has also reported a "greatly increased risk" of PCP when CD4 counts drop below 200.(8) Numerous other studies have found similar associations between lowered CD4 counts and increased risk of PCP and other opportunistic infections.(6,9,10) Such findings formed the basis for long-standing recommendations regarding opportunistic infection prophylaxis (using drugs to prevent these infections). Other research relevant to this discussion is covered in the section on viral load, below. Regarding the effect of treatment-induced increases in CD4 on clinical prognosis, the small increases seen in Concorde indeed did not correlate with improved long-term outcome. But numerous other studies do show a strong correlation with lowered risk of AIDS-defining opportunistic infections or death, particularly with larger, HAART-induced CD4 increases. In the U.S.-government trial ACTG 320 (which compared AZT plus 3TC vs. AZT plus 3TC plus indinavir [Crixivan(R)]), the indinavir group had a mean CD4 increase roughly three times that of the AZT/3TC only group, and half as many AIDS- defining events.(11) In a meta-analysis (combined analysis) of seven (mostly pre-HAART) antiretroviral studies, researchers found that "having either a reduction in HIV-1 RNA level or an increase in CD4+ lymphocyte count, or both, was associated with a delay in clinical disease progression."(12) Overall, a large body of evidence involving both treated and untreated patients shows a clear correlation between low or declining CD4 counts and increased risk of opportunistic infections or death.(13,14) The denialist view of CD4 counts is used to call into question the 1993 revision of the CDC's AIDS case definition, which added a CD4 count of 200 or lower as an AIDS-defining condition. In Maggiore's words, it "allows HIV-positives with no symptoms or illness to be diagnosed with AIDS. Since 1993, more than half of all newly diagnosed AIDS cases are counted among people who are not sick."(3) The mass of evidence showing that HIV-infected individuals with CD4 counts below 200 are at overwhelmingly increased risk for life-threatening infections is simply ignored. And on Viral Load
Denialist objection to viral load testing is bolstered by the fact that Kary Mullis, who won a Nobel prize for developing the basic technique of PCR, is a supporter of their cause and has questioned the use of his technique to quantify virus.(3) In a 1996 article published in the denialist journal Reappraising AIDS, authors Christine Johnson and Paul Philpott demonstrate their scorn for viral load measurements in the title of their discussion, "Viral Load of Crap." Focusing on the 1995 Ho and Shaw Nature papers on viral dynamics, they write: "Ho and Shaw's technique looks for HIV RNA, the genetic material found in the viral core. They assume that since each HIV contains two HIV RNAs, there must be one HIV for every two HIV RNAs they count. But the large amount of HIV RNA they report is found only after sending blood samples through polymerase chain reactions (PCR). PCR is the 'DNA fingerprinting' technology which takes tiny numbers of genetic molecules (RNA or DNA) and turns them into huge quantities." What these tests find, they argue, is meaningless: "Some of these are HIVs that have been neutralized by antibodies, some are defective HIVs (those that did not form correctly) and some are free-floating HIV RNA. Though none of these entities has any pathological capacity, the viral load technique confuses them with whole, infectious virus, the only kind that has any biological significance."(16) This essay is typical of the denialist analysis of viral load, illustrating both its strengths and weaknesses. Like much of the movement's literature, they discuss only PCR and not the other technologies used to quantify viral load, mistakenly stating that Ho used PCR when in fact he used bDNA (branched DNA)--a different process marketed by a different company.(17,18) Philpott and Johnson effectively lay out the theoretical reasons why PCR-based viral load tests might produce a misleading result. Indeed, company researchers and the FDA have acknowledged potential causes of error and variation in viral load results, and a potential margin of error in these assays of roughly threefold.(18,19) Thus, when the FDA approved the Roche Amplicor HIV-1 Monitor (a PCR-based assay), it required the labeling to indicate that the test can accurately detect a three-fold or greater change in HIV RNA for patients with a viral load of 1000 copies or greater and a six-fold or greater change for patients whose viral load is below 1000.(19) (Although Maggiore is correct in saying that the FDA has not approved PCR for diagnosing HIV infection, she neglects to mention that the agency did approve it "to assess patient prognosis... or to monitor the effect of antiviral therapy"). Strikingly, Philpott and Johnson stick entirely to theory and do not address the key question of whether or not viral load measurements predict the likelihood of disease progression or death in the real world. A very large body of evidence indicates they do, some of which was available prior to their dismissal of the tests as a "Viral Load of Crap." The mass of confirming data--from ongoing cohort studies as well as antiretroviral trials--that has accumulated since then is rarely acknowledged in denialist writings. Beginning in 1995 John Mellors and colleagues published a series of articles detailing MACS cohort data showing a strong correlation between baseline viral load and subsequent disease progression.20,21,22 Using stored blood samples from patients' early study visits, Mellors examined the rates of AIDS-defining events and deaths in relation to viral load levels measured using bDNA. In a 1604-patient sample, only 0.9 percent of those whose baseline viral load was 500 copies or lower died of AIDS within six years, while 69.5 percent of those whose viral load was greater than 30,000 copies died. "Plasma viral load was the single best predictor of outcome," Mellors wrote, "followed by CD4+ lymphocyte counts [T-cell counts] and neopterin levels, beta2-microglobulin levels, and thrush or fever. We observed a strong association between viral load and the subsequent rate of decline in CD4+ lymphocyte counts."(22) Similarly strong associations between viral load levels and clinical outcome have been reported in numerous other cohort studies, including the 1170-patient EuroSIDA cohort(23) and the Multicenter Hemophilia Cohort Study,(24) among others. In the hemophilia cohort, "each log(10) increase in baseline viral load was associated with a five-fold increase in risk for AIDS-related illness during the first six months of follow-up." The predictive value of viral load was independent of that of CD4 count. One particularly interesting study looked at viral load in gay men in the Baltimore MACS cohort and injection drug users in the Baltimore "AIDS Link to Intravenous Experiences" (ALIVE) cohort. Rather than measuring plasma HIV-RNA in the usual way, using PCR or bDNA, this study looked at cell- associated infectious viral load using the quantitative microculture assay. This method "quantifies the biologically functional and infectious cell-associated HIV-1 by measuring the amount of HIV infected cells capable of infecting donor cells from an uninfected person in culture."(25) Looking at the risk of AIDS-defining infections, non-AIDS-defining bacterial infections, and death, the researchers found that "higher levels of infectious viral load were significantly related to increased hazards for all three outcomes," with little difference between the gay men and the intravenous drug users. After adjusting for CD4 level and numerous other factors, viral load was strongly predictive of risk of progression to AIDS. The association between viral load (measured using bDNA or PCR) and clinical progression has been seen consistently in HIV treatment trials, including the meta-analysis of seven studies discussed above,(12) in which "each 10-fold decrease in HIV-1 RNA was associated with a 51 percent reduction in progression risk." In both the pivotal trial of ritonavir(26) and ACTG 320,(11) patients randomly assigned to the protease inhibitor arm showed significantly better suppression of viral load and significantly reduced AIDS-defining events. After reviewing the available data, including numerous studies not listed here, the expert panel convened by the Department of Health and Human Services to determine HIV treatment guidelines recommended using both CD4 and viral load in conjunction with the clinical condition of the patient to guide therapeutic decision-making. The panel noted, "Multiple analyses in over 5,000 patients who participated in approximately 18 trials with viral load monitoring showed a statistically significant dose-response type association between decreases in plasma viremia and improved clinical outcome."(27) Discussion of this data is notably absent even in current denialist literature. Maggiore's recent column,(15) for example, cites one article from 1993(28)--very early in the development of these assays--as "studies showing that viral load test results do not correlate with illness, with wellness, with T-cell counts or even the finding of virus by co-culture." This is at best a dubious interpretation of this study, and Maggiore fails to discuss any of the more recent evidence showing precisely the opposite. Evidence cited of viral loads found in HIV-negative people turns out to be a handful of anomalous cases, several of which involve false- negative antibody tests in people who clearly had AIDS.(29) Evaluating the Evidence No lab test or surrogate marker is perfect. All have innate limitations, natural variation, and a chance of error, and as a result HIV/AIDS researchers and treatment activists alike have cautioned that physicians must always remember they are treating patients, not lab values. The limitations of CD4 and viral load tests, both real and theoretical, have been exhaustively described by the denialists. But their declarations that these tests are meaningless are based on a skewed, highly selective reading of the data that simply omits anything which might contradict their views. The overwhelming preponderance of evidence strongly indicates that both CD4 and viral load measurements can provide useful and important information that doctors and patients can use to evaluate progress and make treatment decisions. For More Information Many of the denialist Web sites and books are accessible through the references below. Unfortunately, the medical mainstream has usually not bothered to answer these views--so persons with sincere questions have heard only one side. This is changing. Meanwhile, the U.S. National Institute of Allergy and Infectious Diseases has prepared a page of links to publications with evidence that HIV causes AIDS, http://www.niaid.nih.gov/spotlight/hiv00/default.htm . Also, see http://www.aegis.org/topics/aids_debate.html . References 1. ACT UP Hollywood home page, www.outspoken.org/actuphollywood/index.html 2. Strausberg, John. The AIDS Heretics, New York Press. March 9, 2000; 13: 10. 3. Maggiore, Christine. What if Everything You Thought You Knew About AIDS was Wrong? (4th Edition, 2000). American Foundation for AIDS Alternatives, Studio City, California. 4. Conlan, Mark Gabrish. Interview: John Lauritsen.Zenger's. April 1997. 5. Mosley, James. Idiopathic CD4+ Lymphocytopenia: Other Lymphocyte Changes. IX International Conference on AIDS, Berlin, 1993, abstract #WS-A25-5. 6. Stein, Daniel S, Korvick, Joyce A. and Vermund, Sten H. CD4+ Lymphocyte Cell Enumeration for Prediction of Clinical Course of Human Immunodeficiency Virus Disease, a Review. Journal of Infectious Diseases, 1992; 165: 352-363. 7. Stansell, J.D., and others. Predictors of Pneumocystis carinii pneumonia in HIV-infected persons. Pulmonary Complications of AIDS Study Group. American Journal of Resperitory and Critical Care Medicine. January 1997; 155:1, 60-66. 8. Phair, J., and others. The risk of Pneumocystis carinii pneumonia among men infected with human immunodeficiency virus type 1. Multicenter AIDS Cohort Study Group. New England Journal of Medicine. January 1990; 322:3, 161-165. 9. Nightingale, SD, and others. Incidence of Mycobacterium avium-intracellulare complex bacteremia in human immunodeficiency virus-positive patients. Journal of Infectious Diseases. June 1992; 165: 6, 1082-1085. 10. Spaide, R.F., Gaissinger, A., and Podhorzer, J.R. Risk factors for cotton-wool spots and for cytomegalovirus retinitis in patients with human immunodeficiency virus infection Ophthamology. December 1995; 102:12, 1860-1864. 11. Hammer, S., and others. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic milliliter or less. New England Journal of Medicine, 1997; 337: 725-733. 12. Marschner, I. C., and others. Use of Changes in Plasma Levels of Human Immunodeficiency Virus Type 1 RNA to Assess the Clinical Benefit of Antiretroviral Therapy. Journal of Infectious Diseases. 1998; 177: 40-47. 13. Smith, D.K., and others. Causes and rates of death among HIV-infected women 1993-1998: The contribution of illicit drug use and suboptimal HAART use. 7th Conference on Retroviruses and Opportunistic Infections, San Francisco, January 30-February 2, 2000, abstract #682. 14. O'Brien, William A., and others. Changes in plasma HIV RNA level and CD4+ lymphocyte counts predict both response to antiretroviral therapy and therapeutic failure. Annals of Internal Medicine. 1997; 126: 939-945. 15. Maggiore, Christine, Questioning AIDS, Q & A. Magnus. March/April, 2000. 16. Johnson, Christine and Philpott, Paul. Viral Load of Crap. Reappraising AIDS. October, 1996. 17. Ho, D.D., and others. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature. January 12, 1995; 373: 123-126. 18. Todd, J. Performance Characteristics for the quantitation of plasma HIV-1 RNA using the branched DNA signal amplification technology.Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1995; 10: supplement 2, S35-44. 19. Food and Drug Administration, letter to Roche Molecular Systems, March 2, 1999. 20. Mellors, J., and others. Quantitation of HIV-1 RNA in plasma predicts outcome after seroconversion. Annals of Internal Medicine. 1995; 122: 573-579. 21. Mellors, J., and others. Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science. May 24, 1996; 272: 1167-1170. 22. Mellors, J., and others. Plasma viral load and CD4+ lymphocytes as prognostic markers in HIV-1 infection. Annals of Internal Medicine. 1997; 126: 946-954. 23. Miller, V., and others. Association of viral load, CD4 cell count, and treatment with clinical progression in HIV patients with very low CD4 cell counts: The EuroSIDA cohort. 7th Conference on Retroviruses and Opportunistic Infections, San Francisco, January 30-February 2, 2000, abstract #454. 24. Engels, E., and others. Plasma HIV-1 viral load in patients with hemophilia and late-stage HIV disease: A measure of current immune suppression .Annals of Internal Medicine. 1999; 131:256-264. 25. Lyles, C.M., and others. Cell-associated infectious HIV-1 load as a predictor of clinical progression and survival among HIV-1 infected injection drug users and homosexual men. European Journal of Epidemiology. 1999, 15:99-108. 26. Cameron, D.W., and others. Randomized placebo-controlled trial of ritonavir in advanced HIV-1 disease. The Lancet. February 21, 1998; 321: 543-549. 27. Panel on Clinical Practices for Treatment of HIV Infection. Guidelines for the Use of Antiretroviral Agents in HIV-infected Adults and Adolescents. January 28, 2000. (This document is available at http://www.hivatis.org .) 28. Piatak, M, and others. High levels of HIV-1 in plasma during all stages of infection determined by competitive PCR. Science. March 1993; 259: 1749-1753. 29. Sullivan, P.S., and others. Persistently negative HIV-1 antibody enzyme immunoassay results for patients with HIV-1 infection and AIDS: serologic, clinical and virologic results. Seronegative AIDS Clinical Study Group. AIDS. January 1999; 12:1, 89-96. AIDS Treatment News Published twice monthly Subscription and Editorial Office: P.O. Box 411256 San Francisco, CA 94141 800/TREAT-1-2 toll-free U.S. and Canada 415/255-0588 regular office number Fax: 415/255-4659 E-mail: aidsnews@aidsnews.org
Editor and Publisher: John S. James Associate Editor: Tadd T. Tobias Reader Services: Tom Fontaine and Denny Smith Operations Manager: Danalan Richard Copeland Statement of Purpose: AIDS Treatment News reports on experimental and standard treatments, especially those available now. We interview physicians, scientists, other health professionals, and persons with AIDS or HIV; we also collect information from meetings and conferences, medical journals, and computer databases. Long-term survivors have usually tried many different treatments, and found combinations which work for them. AIDS Treatment News does not recommend particular therapies, but seeks to increase the options available. Subscription Information: Call 800/TREAT-1-2 Businesses, Institutions, Professionals: $270/year. Includes early delivery of an extra copy by email. Nonprofit organizations: $135/year. Includes early delivery of an extra copy by email. Individuals: $120/year, or $70 for six months. Special discount for persons with financial difficulties: $54/year, or $30 for six months. If you cannot afford a subscription, please write or call. Outside North, Central, or South America, add air mail postage: $20/year, $10 for six months. Back issues available. Fax subscriptions, bulk rates, and multiple subscriptions are available; contact our office for details. Please send U.S. funds: personal check or bank draft, international postal money order, or travelers checks. ISSN # 1052-4207 Copyright 2000 by John S. James. |

© 1997-2000 BEI
 AIDS dissidents from ACT UP/San Francisco protesting in Atlanta
AIDS dissidents from ACT UP/San Francisco protesting in Atlanta 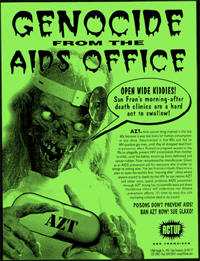 A protest flyer against AZT treatment from ACT UP/San Francisco AIDS dissidents
A protest flyer against AZT treatment from ACT UP/San Francisco AIDS dissidents